Overactive bladder, or irritable bladder, is a condition in which individuals experience sudden, involuntary contractions of the muscles in the wall of the urinary bladder, creating a sudden, involuntary need to urinate. This spontaneous episode of urinary urgency can occur even if you have only a small amount of urine in your bladder.
Millions of men and women have overactive bladder, but it is also a condition few people admit they have, even to their doctors. Yet according to a new study (May 2011) published in Urology that involved 20,000 men and women, an estimated 29.8 million adults aged 40 years or older in the United States have bothersome symptoms of overactive bladder.
Overactive bladder is a type of urinary incontinence, which is why another name for the condition is urge incontinence. Urge incontinence differs from another type of incontinence—stress incontinence—which is the most common type. Stress incontinence occurs when there is a weakness in the structures that prevent the bladder from leaking urine. People with stress incontinence leak urine when they sneeze, laugh, lift, or participate in certain physical activities. An overactive bladder has a different cause.
Causes of Overactive Bladder in Men
An overactive bladder is caused by a malfunction in the nerves and muscles of the bladder, which causes the bladder muscles to spasm, resulting in an urge to urinate. In a well-functioning bladder, the detrusor muscle (a major muscle of the bladder) contracts in response to filling of the bladder with urine. The nervous system regulates the contraction and relaxation of the detrusor muscle. A normal adult bladder can hold up to 600 cc of urine. When about 300 cc of urine is in the bladder, the nervous system sends a signal to trigger the bladder muscles to coordinate urination. However, a healthy individual has voluntary control over the sphincter muscles at the opening of the bladder and can hold the urine for a longer time.
When an individual has an overactive bladder, however, the detrusor muscle contracts at inappropriate times, regardless of how much urine is in the bladder. Nervous system conditions that can cause overactive bladder include spinal cord injury, Parkinson’s disease, dementia, multiple sclerosis, diabetic neuropathy, and stroke. Other conditions or situations not related to a nervous system disorder that can cause overactive bladder include prostate surgery, BPH, bladder stones, bladder tumors, external radiation for prostate cancer, use of certain medications such as diuretics or hypnotics, prostatectomy (if the nerves have been damaged), and urinary tract infections.
In some cases, no cause is ever identified (idiopathic overactive bladder). Although about 40 percent of people age 75 and older have symptoms of overactive bladder, the condition is not considered to be a normal part of aging.
Symptoms of Overactive Bladder in Men
The symptoms of an overactive bladder include
- urinary urgency (sudden, strong need to urinate immediately)
- frequent urination (the need to void 8 or more times during a 24-hour period)
- urinating in the middle of the night (2 or more times; nocturia)
- urge incontinence (an inability to stop urine leakage that follows a sudden, strong urge to urinate)
These symptoms can cause a significant amount of psychological stress and affect men’s social, physical, occupational, and sexual activities.
In a study of overactive bladder that involved 9,416 men and 10,584 women, the investigators uncovered the following information about symptoms and how they affected the study participants:
- Symptoms of overactive bladder occurred at least “sometimes” in 27.2% of men and 43.1% of women
- Symptoms occurred at least “often” in 15.8% of men and 32.6% of women
- Among men who had symptoms sometimes, 60% said they were bothered “somewhat” and 27.8% said they were bothered “quite a bit.”
- Among men who had symptoms often, 67.8% said they were bothered “somewhat” and 38.2% said they were bothered “quite a bit”
Clearly, overactive bladder can be a disruptive factor in the lives of millions of adults.
Diagnosis of Overactive Bladder in Men
To diagnose overactive bladder, your doctor will ask you about your urinary habits, what symptoms you have been experiencing, and whether you have any neurological condition. You should also be questioned about your dietary habits to see if you are eating foods that could irritate your bladder. This information, along with whatever your doctor uncovers after performing any of the following tests, can help lead to a diagnosis.
- A digital rectal exam (DRE) is a standard test to help identify any problems with the prostate gland, which could be a factor in overactive bladder. A DRE involves your doctor inserting a gloved, lubricated finger into your rectum and pressing on the prostate to feel for any abnormalities in size or shape.
- A urinalysis involves taking a urine sample, which your doctor will have examined to see if you have any signs of infection or other problems; for example, the presence of red blood cells indicate bleeding in the urinary tract, proteins is a sign of a kidney problem, while white blood cells indicate a urinary tract infection.
- An ultrasound of the bladder may be done to identify how much urine is left in the bladder after you urinate (called post-void residual) and help your doctor determine if there is an obstruction or weak bladder muscles.
- A uroflowmeter is an instrument that measure urine flow rate. You will be asked to urinate into the device, which translates the information into a graph of changes in flow rate, the amount of urine you void from your bladder, and flow time.
- Cystometry is a test that measures the amount of pressure in the bladder during filling. One catheter is used to fill your bladder slowly with water while another one containing a pressure sensor is placed in your rectum. This test can detect involuntary muscle contractions and the level of pressure at which you feel the urge to urinate or experience leakage.
- Electronomyography measures bladder nerve impulses. Sensors are placed either on or in the skin in your pelvic floor, and they detect nerve impulses in your bladder muscles and urinary sphincter.
- During a cystoscopy, your doctor inserts a long thin tube into your penis through the urethra until it enters the bladder. The cystoscope has a tiny lens that allows your doctor to see inside your bladder and urethra. He or she can look for abnormalities such as bladder stones or tumors, determine how strongly the prostate is squeezing the urethra, and see if there is any urine remaining in the bladder after voiding.
Treatment for Overactive Bladder in Men
Medical treatment for overactive bladder includes medications, noninvasive medical procedures, behavioral therapies, and surgery. Overall, the good news is that the estimated success fate of treatment with a combination of medications and behavioral therapies is about 80 percent.
Overactive bladder that is not treated or treated ineffectively can result in urinary tract infections, skin irritation and/or skin infections (from urine leakage and from wearing adult diapers and/or pads), and formation of bladder stones. Falls and fractures are possible complications in the elderly.
Medications for Overactive Bladder
The most common medications used to treat overactive bladder are called anticholinergics, which can decrease the activity of the detrusor muscle. Anticholinergics have a host of common side effects, including blurry vision, confusion (mostly in the elderly), constipation, double vision, dry mouth, loss of coordination, sensitivity to light, and urinary retention, among others. Medications used to treat overactive bladder include the following:
- Darifenacin (Enablex), a recent addition to the anticholinergic class, is most helpful in elderly patients who have dementia, because it is less likely to cause confusion, a common side effect of anticholinergics.
- Fesoterodine fumarate (Toviaz) is indicated for overactive bladder patients who have urge incontinence, urgency, and frequency. The drug is taken once daily.
- Oxybutynin (Ditroopan) helps prevent urge incontinence by relaxing the detrusor muscle. The regular form is taken 2 to 3 times daily, while the extended release form (Ditropan XL) can be taken once daily. A patch (Oxytrol) is also available, but it releases a smaller dose than the oral form.
- Solifenacin (VESIcare) is another newer addition to the anticholinergic line and is similar to tolterodine and is taken once daily.
- Tolterodine (Detrol, Detrol LA) helps with symptoms of urinary frequency, urgency, and urge incontinence, and has less impact on the salivary glands than does oxybutynin and is better tolerated. Detrol is taken twice daily, while Detrol LA is taken once.
In addition to anticholinergics, there are several other medication options you and your doctor may consider.
- Tricyclic antidepressants (e.g., doxepin [Sinequan], imipramine [Tofranil]) are also sometimes prescribed for overactive bladder. Side effects may include blurry vision, changes in appetite, dizziness, and dry mouth.
- Alpha-blockers. This class of drugs is typically used to treat BPH. They work by relaxing the smooth muscles of the prostate and bladder neck, which then allows normal urine flow and prevents abnormal bladder contractions that can lead to urge incontinence. Drugs in this class include alfzosin (Uroxatral), doxazosin (Cardura), tamsulosin (Flomax), and terazosin (Hytrin). Side effects include dizziness, fatigue, and headache.
- Botox. In August 2011, the Food and Drug Administration (FDA) approved the use of Botox for overactive bladder caused by neurologic disorders such as multiple sclerosis and spinal cord injuries.
Nerve Stimulation for OAB
Tibial nerve stimulation is a medical procedure that can help individuals who have not responded to medications or other nonsurgical options and who don’t want to undergo surgery. The procedure involves placing a needle through the skin near your ankle until it reaches the tibial nerve (a nerve in the leg). An electric impulse is sent through the needle, and the signals travels along the tibial nerve to the spine and makes contact with the nerves that control the bladder. You will need to have about 12 treatments, one per week, and each session takes about 30 minutes.
Surgical Procedures
Surgery is rarely necessary to treat overactive bladder. However, if your symptoms are seriously disrupting your quality of life and you have not responded to other treatments, your doctor may recommend a minor surgical procedure called sacral nerve stimulation, or a major surgical procedure, cystoplasty, also known as bladder augmentation.
- Sacral nerve stimulation involves surgically implanting a pacemaker-like device called a stimulator under the skin, usually in the buttocks. This device sends mild, electrical impulses to the nerves that control urination. The surgery can be done as an outpatient procedure under local anesthesia and mild sedation. Once the device has been implanted, you will need to limit your physical activities (including sex) for three weeks or longer until your incisions heal completely. You will have a handheld control instrument you can use to adjust the level of stimulation. The stimulation is painless and can be highly successful for people who have not had success with medication or lifestyle changes.
- Cystoplasty is major abdominal surgery and involves a surgeon using a piece of tissue from your stomach or intestines to enlarge your bladder. Many men require use of a catheter for the rest of their lives after the procedure. Once you leave the hospital, it typically takes six weeks or longer to return to a normal schedule. Bladder augmentation does not always cure overactive bladder, and infection can be a complication.
Behavioral Therapies
One of the most effective ways to treat overactive bladder is to improve pelvic muscle tone, which helps prevent leakage. You can strengthen your pelvic muscles in several ways, both with and without the need for any devices.
- Kegel exercises. These pelvic muscle exercises can be done while you are sitting in a chair, standing in line, watching TV…and no one will even know you are doing them. Kegel exercises involve squeezing the muscles you would use if you were trying to stop from passing gas. These exercises can strengthen the pelvic floor muscles and urethra, which can support the bladder opening to prevent leakage. For best results, Kegel exercises should be done daily, at least 3 to 4 sets of 8 to 12 contractions for at least eight weeks.
- Biofeedback. When used along with Kegel exercises, biofeedback has been shown to help people better control and become more aware of their pelvic muscles.
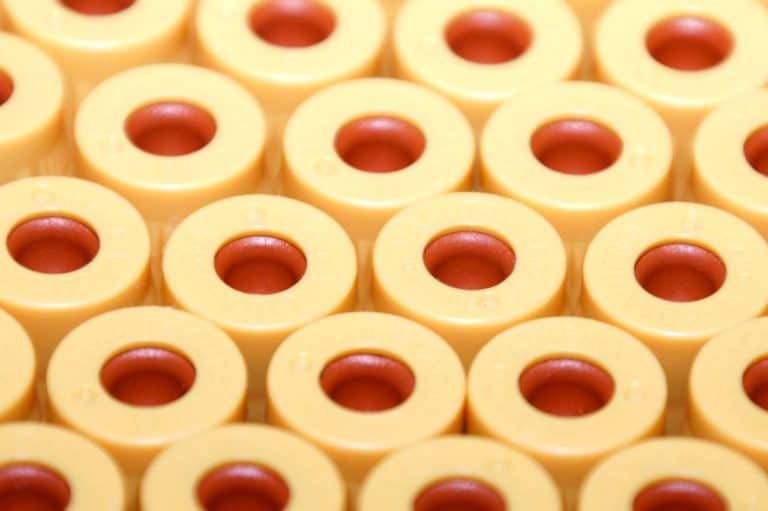
- Pelvic-floor electrical stimulation. This treatment requires use of a device that delivers very mild electrical pulses to stimulate muscle contractions in the pelvic floor. You can do the therapy yourself at home using the electrostimulation device with an exerciser that is inserted into your rectum. You control the amount of stimulation with a control device. Electrical stimulation can be used along with Kegel exercises.
- Bladder training. This is a technique in which you learn how to resist your urge to void and gradually extend the time between voiding. Bladder training may also include scheduled toileting (going to the bathroom at predetermined times, even if you don’t feel like you need to void), keeping a diary of your urination and leakage episodes, and Kegel exercises.
OAB/Incontinence Products and Devices for Men
Continence products such as adult diapers, absorbent pads, penile clamps, or compression rings can be used to help manage leakage, but technically are not a form of treatment. Absorbant products can be helpful while using medications and other therapies or if treatments have not worked. Care should be taken when using adult diapers or absorbant pads because they can cause skin irritation and/or skin infections.
Penile clamps are cushioned devices that are placed over the penis to prevent urine leakage. Compression rings are placed around the penis and inflated to prevent leakage. Men who use either of these products must remove them every 2 to 3 hours so they can empty their bladder. Penile clamps and compression rings can also damage the penile and urethral tissue if they are not used correctly, as well as slow the development of muscle control necessary to regain urinary continence.
Herbal Remedies For Overactive Bladder
When it comes to using herbal remedies traditionally used to treat overactive bladder, “whether or not they work, I don’t know.” That’s the word from Geovanni Espinosa, ND, Lac, CNS, director of the Integrative Urological Center at New York University’s Langone Medical Center, and a specialist in alternative and naturopathic treatments for urinary tract disorders. The problem, he says, is that “you don’t know exactly how they work until they’re looked at scientifically,” and such studies need to be done.
That said, some herbal remedies are advertised as being specifically for overactive bladder. These remedies come as single ingredient or multi-ingredient formulations. Espinosa notes that combining various herbs is believed to provide a synergistic effect.
Despite the lack of scientific studies in humans to support any beneficial claims, the following herbal remedies are sometimes used to manage overactive bladder symptoms. Check with your healthcare provider before taking any of these herbal remedies.
- Buchu (Barosma betulina). Bucha is a South African plant that has a history of use for bladder and kidney infections. According to Espinosa, bucha may “nourish the bladder tissue.”
- Cleavers (Galium aparine) is a plant commonly found in the eastern United States and along the Pacific coast. Cleavers is typically added as an ingredient in herbal remedies for treating urinary conditions because the herb is believed to have a diuretic effect. Espinosa explains that cleavers may also help soothe the lining of the bladder wall and protect against irritation.
- Cornsilk (Zea mays) for urinary infections goes back to the time of the ancient Incas. The silky threads of the corn stalk are said to soothe the urinary tract.
- Gosha-jinki-gan is a combination of 11 Chinese herbs. Animal studies suggest the formulation may increase bladder capacity and reduce bladder contractions, while a few small Japanese studies in adults with overactive bladder reported an improvement in symptoms. In one study, 30 older men with overactive bladder showed significant improvement in symptoms after taking gosha-jinki-gan for 6 weeks. (Nishijima 2007; Ogushi 2007)
- Horsetail (Equisetum arvense) is credited with antioxidant, diuretic, and anti-inflammatory properties, and has been used to treat urinary tract infections, urinary incontinence, and kidney and bladder stones.
Dr. Espinosa notes that naturopathic physicians sometimes recommend men take herbs with antioxidant and anti-inflammatory properties to help manage processes that can contribute to overactive bladder. Suggested antioxidants include alpha-lipoic acid, vitamin C, and vitamin E, while anti-inflammatory options may include bromelain, quercetin, and saw palmetto. Other herbal remedies that may be beneficial for urinary tract health in general include cranberry, pollen, probiotics, stinging nettle, and uva ursi.
Diet and Overactive Bladder
If you have an overactive bladder, your first thought may be to limit the amount of fluids you consume so you will not need to use the bathroom as much. Although this sounds like a good idea, if you don’t drink enough fluids (eight cups a day is recommended), your urine can become concentrated, which can actually irritate your bladder and make urge incontinence worse. Therefore, it is important to get enough fluids (e.g., pure water, green tea are best) for good health.
However, not all types of fluids are wise choices when you have overactive bladder, and the same thing holds for some foods. If you have overactive bladder, the following foods and beverages should be avoided, as they can irritate the bladder:
- Citrus fruits and fruit juices (e.g., oranges, grapefruit, pineapple, lemons)
- Coffee and black tea (including decaf)
- Sugar and honey; artificial sweeteners (e.g., aspartame) can bother some people
- Tomatoes and tomato products (they are acidic)
- Spicy foods (e.g., curries, hot peppers, chilies)
- Alcohol
- Chocolate (dark is less irritating than milk chocolate)
- Milk and cheese
- Energy drinks (usually contain caffeine; check the labels)
- Carbonated beverages
Preventing Overactive Bladder
Overactive bladder can be caused by a variety of factors, so it may not be possible to prevent it in all cases. However, there are things you can do to reduce your risk and/or symptoms.
- Get regular, daily exercise
- If you are overweight, losing weight can help with overactive bladder, because excess pounds can exert pressure on the bladder.
- Limit or eliminate your consumption of alcohol and caffeine.
- Avoid spicy foods, citrus fruits and beverages, sugar, honey, tomato products, and chocolate (if you must have chocolate, choose dark rather than milk chocolate).
- Quit smoking
- Do Kegel exercises every day if you have overactive bladder, or at least 3 to 4 times a week to help prevent it.
- Manage any chronic condition, such as diabetes, that can contribute to overactive bladder
- Don’t hold it! Use the bathroom whenever you feel the urge.
- Promptly treat any urinary tract infections
- Avoid constipation, which can place stress on the bladder
References
Coyne KS et al. National community prevalence of overactive bladder in the United States stratified by sex and age. Urology 2011 May; 77(5): 1081-87
Nishijima S et al. Effect of gosha-jinki-gan, a blended herbal medicine, on bladder activity in rats. J Urol 2007 Feb; 177(2): 762-65
Ogushi T, Takahashi S. Effect of Chinese herbal medicine on overactive bladder. Hinyokika kiyo 2007 Dec; 53(12): 857-62