Americans are living longer. In 2014, USA Today reported a new record high for life expectancy. Today, according to the Centers for Disease Control and Prevention, the average person will live to be 78.8 years old (for women, 81.2 years; for men, 76.4 years). Heart disease remains the number one cause of death, and cancer is number two.
Increased life expectancy has many implications. A big one for prostate cancer patients who seek treatment is the need to consider the likelihood of late-onset side effects (those that may not show up for years) as well as long term side effects that can lessen quality of life. For treatments that either remove the prostate (radical prostatectomy) or immediately destroy the cancer inside the gland (thermal ablation using extreme heat or cold) side effects–if they occur–usually happen immediately but may improve over time.
For example, a study of very low risk prostate cancer patients who had robotic surgery found that by 12 months after surgery, 84% of the men were continent (<1 pad every 24 hours) and 44% were capable of erectile function. “The proportion of men achieving the trifecta, defined as preoperative potent and continent men who remained potent and continent with no BCR [biochemical recurrence] was 38%…at 12 months.” These numbers represent improvement/recovery of function experienced over the year after treatment.
A 60-year-old patient who can reasonably expect to live for another 16.4 years must consider his probable quality of life following treatment. While side effects can be embarrassing or annoying, knowing they will probably improve can make them bearable. This is encouraging for those who lean toward prostatectomy, whether open, laparoscopic, or robotic.
On the other hand, a more discouraging possibility accompanies radiation treatment for prostate cancer. Many men are drawn to noninvasive radiation, despite weeks of daily treatment or permanent radioactive seed implants, because there are so few risks of immediate side effects. However, radiation does not kill cancer instantly, as thermal ablation does, but rather interferes with the cancer cells’ ability to reproduce themselves. This requires continuous exposure to radiation over time. At the same time, the scatter effect of radiation begins to damage nearby healthy tissues, and this is the source of late-onset side effects like urinary, sexual and bowel problems.
Radiation poses a darker late-onset threat to a patient’s health: the development of secondary cancers. It is well established that the risk of bladder, rectal and colon cancers increases following prostate cancer radiation. Now leukemia must be added to the list. A new study points to a type of cancer of the blood and bone marrow in which immature white blood cells proliferate. It is called acute myeloid leukemia (AML), and the accumulation of excess white blood cells in the bone marrow interferes with the production of normal blood cells. According to www.cancer.gov, exposure to radiation is one of the causes of adult AML.
A new prostate cancer study by Wang et al (Nov. 2016) reported, “Compared with elderly patients with prostate cancer (PCa) receiving surgery only, those receiving radiotherapy (RT), especiallly intensity=modulated radiotherapy (IMRT), had an increased risk of…acute myeloid leukemia (AML).” While the overall incidence for radiation therapy patientsis low (1.2%), it is nearly twice the incidence of those who had surgery only (0.7%). Also, patients who had IMRT (intensity modulated radiation therapy) developed AML earlier (median 2.28 years) than those who had brachytherapy (median 3.78 years) or conventional external beam radiation (4.17 years). AML is difficult to treat once it has progressed, so it is important that it be diagnosed early when it may still be curable.
As we look forward to longer lifespans, men who develop prostate cancer–or any cancer–are urged to thoroughly consult with their doctors about the side effects of the treatments for which they are qualified. In addition, second opinions are always advisable, and thanks to the abundance of information on the internet, web-based research can shed additional light. It would be a cruel irony to undergo a treatment that succeeded in controlling one cancer, only to have it associated with the risk of another that might be more deadly.
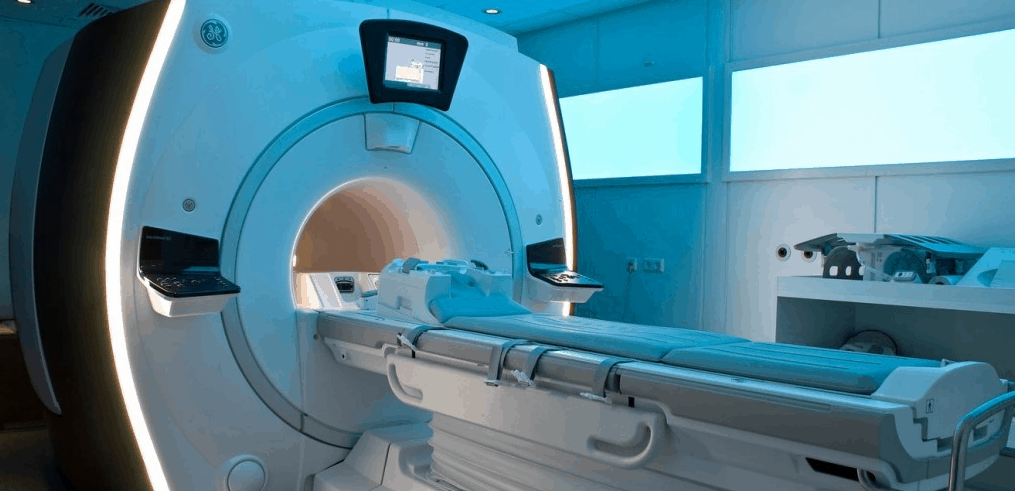
For patients who qualify for a focal treatment, Focal Laser Ablation (FLA) is a safe, highly effective MRI-guided treatment that targets just the tumor, but spares urinary and sexual function. It is repeatable if necessary, and it leaves all future treatment options open if cancer comes back. The Sperling Prostate Center offers advanced 3T multiparametric MRI and MRI-guided targeted biopsy, the most sophisticated technology for diagnosing prostate cancer, and determining if a patient qualified for FLA. Our diagnostics also help men match their cancer with the ost strategic treatment options, including active surveillance. For more information visit www.sperlingprostatecenter.com.
Copyright by Dan Sperling, MD. Reprint permission courtesy of Sperling Prostate Center (New York, Florida), the leading U.S. center for multiparametric detection, diagnosis and image-guided focal treatment of prostate cancer.
Read more in our Prostate Cancer Health Center.
References
Carlsson S et al. Oncological and functional outcomes 1 year after radical prostatectomy for very-low-risk prostate cancer: results from the prospective LAPPRO trial. BJU International 2016 Aug; 118(2): 205-12
Copeland L. Life expectancy in the USA hits a record high. USA Today Oct 9, 2014
Wang R et al. Myelodysplastic syndromes and acute myeloid leukemia after radiotherapy for prostate cancer: a population-based study. Prostate 2017 Apr; 77(5): 437-45