General Tests for Prostatitis–What to Expect

Medically reviewed by Dr. Paul Song M.D
Article at a Glance
- When testing for prostatitis, the doctor should perform a full physical exam.
- One of the basic tests is the National Institute of Health’s Chronic Prostatitis Symptoms Index (CPSI).
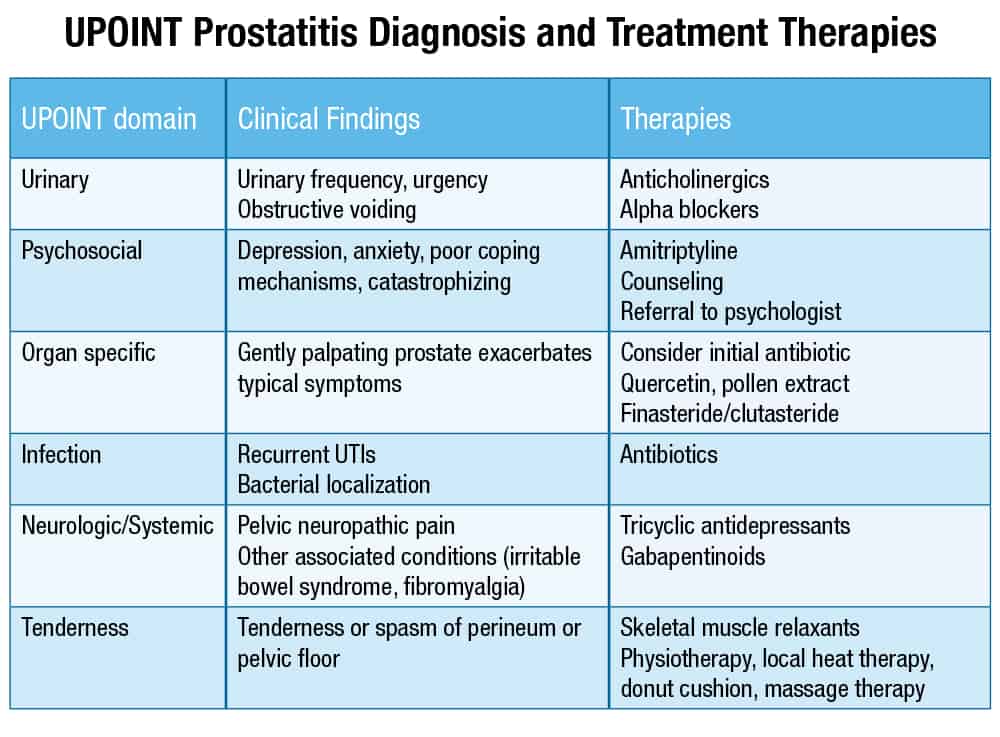
- UPOINT is a system that doctors can use to make effective treatment decisions for CPPS patients.
There are several general tests for prostatitis that your doctor may order or perform when trying to diagnose your type of prostatitis. Here’s an idea of the general tests and what you can expect at the doctor’s office when you are in the process of diagnosing prostatitis.
Because there are many conditions and diseases that have symptoms similar to prostatitis, it is important to undergo a full examination. Getting the right diagnosis and determining what type of prostatitis you have is key to starting the right treatments. Your doctor should conduct a physical examination. That includes examining your external genitalia, scrotum, perineum, and prostate as well as other nearby areas of your body. He or she should also examine your abdomen, flank (which is the side of your body between the ribs and hip), and your back for signs of inflammation.
Tests for Prostatitis
After the physical exam, your physician will then perform a series of tests (or order other tests) to help make a proper diagnosis. The following include some of the general tests—what to expect:
- Medical history & symptoms test (such as the CPSI)
- Digital rectal examination (DRE), which may detect inflammation of the prostate.
- Prostate specific antigen (PSA) test. The PSA level is often elevated in men who have an inflamed prostate. This test requires a blood sample.
- Urinalysis (a urine sample)—may reveal the presence of white blood cells and bacteria.
- Milking the prostate, also known as prostate massage, which can be used both for both diagnosing and treating prostatitis
- Meares-Stanley “Four Glass Test” involves urine samples
- Pre- and Post-Massage Test (PPMT)—involves taking urine samples before and after prostate massage, which is performed by doctor.
- MRI if doctor needs more information
- Ultrasound if doctor needs more information
- Cystoscopy—a more invasive test that not every patient requires
- Uroflowmetry—a noninvasive test to see the condition and function of your lower urinary tract
- An analysis utilizing UPOINT to classify symptoms to help choose specific treatments
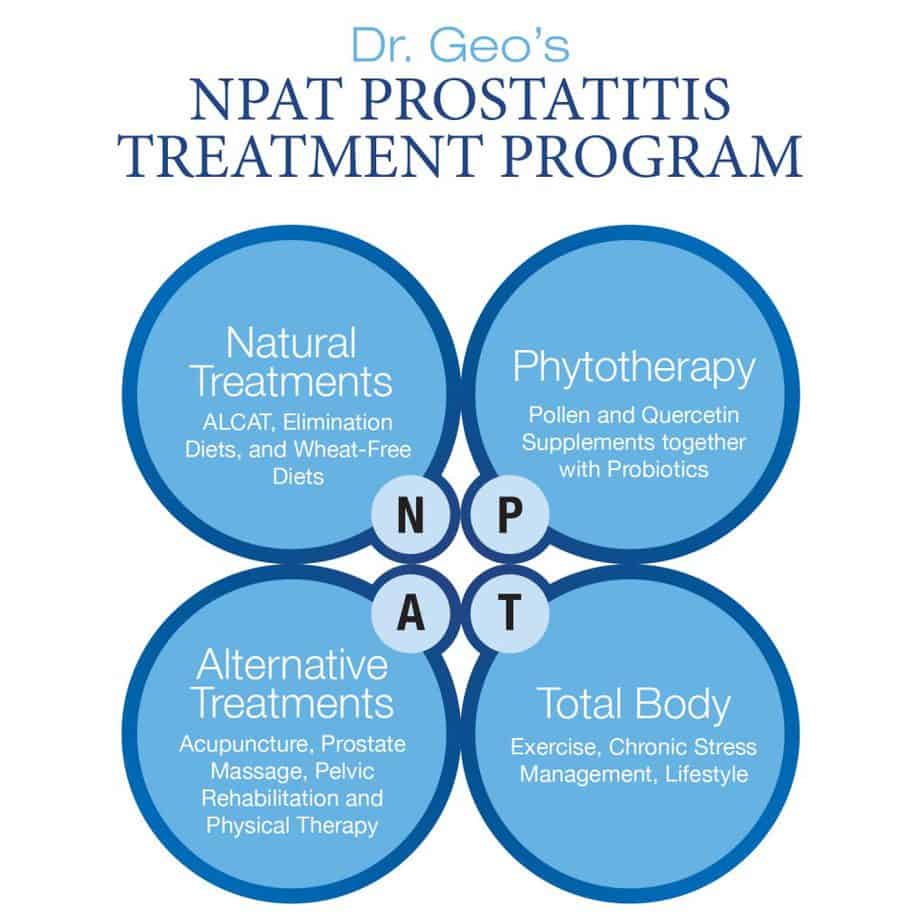
- An analysis of symptoms using the NPAT Prostatitis Program
- Other tests
Medical History & Symptoms Test
One of the first things your physician should do is to take your medical history and to inquire about your symptoms. That process can vary depending on whether you are seeing a familiar family doctor who knows your history well versus seeing this doctor for the first time. If you are visiting a doctor who already has your medical history, you may be asked to update it. It is important to share the following: your surgical history (particularly urologic), any trauma you have experienced, medication you take, and allergies.
Going to the doctor can be stressful and cause all your thoughts to disappear when you hop up on the table. A good plan is to write down important details, symptoms, questions, a list of medications and/or herbal supplements you take, and what you know about your family history in advance and take it in with you. Consider your personal and family medical history before you visit the doctor. Consider the details about your symptoms—how they started, how long they last, when they occur, and exactly what you have been experiencing.
Your doctor will use all the information gathered about your symptoms to help decide which tests to conduct or order. One of the basic tests that clinicians use is the National Institute of Health’s Chronic Prostatitis Symptoms Index (CPSI). The CPSI asks questions about the severity of your pain, where it is located, how symptoms affect your life, urination problems, and sexual health. Your answers to these questions help guide your doctor in monitoring how severe your symptoms are, but the CPSI is not a diagnostic tool.
Digital Rectal Exam
People usually think of the digital rectal examination (DRE) as a routine way to screen for prostate cancer, but it can also help diagnosis prostatitis and chronic pelvic pain syndrome (CPPS). A DRE is not a procedure that any man typically looks forward to, and many uncomfortable jokes have been made about the process, which involves a doctor inserting a lubricated and gloved finger into the anus and rectum to feel the prostate. You can make this more comfortable by relaxing and urinating before the procedure. This helps the doctor get important information about the status of your prostate. For example, by performing a DRE your doctor can determine the size of your prostate and whether there are any abnormalities such as lumps or lesions. The doctor will also check the wall of your lower colon for any inconsistencies.
There are generally two ways to perform a DRE, and if you have a preference you should definitely speak up in advance. Your doctor may tell you to bend forward at the waist and rest your arms on the examination table. The other way is to lie on your side on the table with knees pulled up to the chest. Either way, the entire procedure takes only a few minutes.
Knowing what to expect may help you prepare mentally. Once you are in position, the doctor will insert a lubricated and gloved finger into your rectum. He or she will feel for any abnormalities, including an enlarged prostate (which can have some similar symptoms to prostatitis). The exam may cause you to feel the need to urinate. You may experience some discomfort or mild pain, but if you focus on your breathing and try to release any tension it will make the process easier for you. A person who has an enlarged, infected, or cancerous prostate might feel more significant pain.
You doctor might palpate some surrounding areas such as the muscles to either side of your prostate. If those muscles feel rock hard or if you react when the muscles are palpated, your doctor may have located the source of your pain. If you have tight or sore pelvic muscles, you likely have a pelvic floor spasm, which is the cause in about half the men who have CPPS. Doctors do not always know to look for this muscle tightness, but it is fairly easy to find and treat with pelvic floor physiotherapy.
You should not experience any side effects from having a digital rectal examination. Your doctor will discuss the findings with you, and you can then move on with the examination and testing.
PSA Test
You might associate the prostate specific antigen (PSA) test with its use as a standard screening tool for prostate cancer, but the PSA test blood test can also help diagnosis prostatitis, especially the asymptomatic form of prostatitis, which does not have other symptoms. Some men with prostatitis have an elevated PSA, and an elevated PSA may be the only sign of the rare asymptomatic inflammatory prostatitis. You’ll want to time this test right to get the most accurate reading because some activities can temporarily increase the reading. Schedule the PSA test before you have your digital rectal exam (DRE) because the DRE. You should also avoid other activities (like sexual activity, trauma to the area, or cycling) for a few days before you have your PSA test because they can temporarily affect the numbers.
Urinalysis
Urinalysis is one of the most basic and simple tests your doctor will perform; yet it can provide a wealth of information. This test evaluates a urine sample. You doctor may order urinalysis to look for the presence of bacteria, proteins, and white blood cells. If you have these or other substances that information can help your physicians determine whether you have an infection or something else causing your symptoms.
The urine is examined for appearance, content, and concentration. For example, if the urine looks cloudy instead of clear you might have a urinary tract infection. Finding bacteria in the urine also indicates a urinary tract infection, which is common in men with chronic prostatitis. High levels of protein in urine might indicate kidney disease.
Your physician may ask you to bring a urine sample from home or for you to provide one while you are at the office. In either case, you should use the sterile collection cup supplied by the doctor. To get a urine sample, follow these steps:
- Wash your hands before collecting the urine.
- Clean the area around your genitals and the head of the penis with medicated towelettes.
- Begin to urinate, and after a few seconds, place the collection cup into the urine stream. Collect about 2 ounces of urine.
- Remove the cup from the urine stream and finish urinating into the toilet.
- Place the lid on the collection cup. If you have collected the urine at home, refrigerate it unless you can reach the lab before 30 minutes.
- Make sure to write your name and time of collection on the cup.
A lot of factors can affect the results of the urinalysis from medications to supplements to foods to beverages. That’s another reason to tell your doctor about diet and any drugs and supplements you take. Substances that can affect urinalysis results include diuretics, Dilantin (phenytoin), Rifadin and Rimactane (rifampin), Pyridium (phenazopyridine), vitamin B, beets, blackberries, and rhubarb.
Milking the Prostate
Milking the prostate, also known as prostate massage, is a technique used to improve blood flow to the prostate gland. When your healthcare provider or you (yes, you can learn to do it yourself) perform prostate massage, it helps deliver more nutrients and oxygen to the prostate and assists in eliminating toxins from the gland. You might say that milking does the prostate good as milking moves good stuff in and the bad stuff out. This technique can help both prevent prostatitis and treat it, which is good to know for men with chronic prostatitis who are looking for ways to keep their prostate from flaring up. Milking the prostate is also good for helping treat other prostate conditions like enlarged prostate (benign prostatic hyperplasia, or BPH).
Milking the prostate is a natural way to help diagnose and treat prostatitis. Your doctor can milk the prostate during the diagnostic process. In fact, prostate massage is necessary if you undergo the Pre- and Post-Massage Test (PPMT).
So how is this test done? To milk the prostate, a doctor wears a glove and inserts a lubricated finger into the anus while the patient leans forward, resting his arms on a table. Once the doctor makes contact with the prostate, he or she applies gentle pressure to the gland and massages it. This should not be painful when done correctly. Even though milking the prostate is best done by a doctor when diagnosing prostatitis, men can learn how to milk and massage the prostate themselves if they want to apply this self-treatment for prostatitis at home.
Meares-Stanley “Four Glass Test”
This test is not done as frequently as other tests because it is time-consuming and expensive. The Meares-Stanley “Four Glass Test” does have its positive points in that it can provide important information about the prostate. Doctors can perform a shorter version of the test (such as a three glass test).
Your doctor uses the Meares-Stanley “Four Glass Test” to look at your urine for the presence of bacteria and white blood cells. There are four (three if a shortened version is used) conditions including the first urine released, urine caught midstream, secretions extracted by using prostate massage, and a sample of urine taken after the massage.
Are four glasses necessary? Researchers did a study involving 353 men that compared the results of using the Meares-Stanley “Four Glass Test” against taking just two samples (secretions from the prostate massage and the post-massage urine sample). Between the two tests, nearly 100% of the results were the same. The two-sample test was less effective at finding the bacteria and white cells in all of the men, but it was 100% effective at identifying the type of bacteria and white cells. Study authors concluded that a simpler two-glass test is reasonable for doctors to use when they are first diagnosing prostatitis.
PPMT
The pre- and post-massage test (PPMT) is a simpler, less time-consuming, and less expensive screening test for diagnosing prostatitis when compared to the Meares-Stanley “Four Glass Test.” To conduct the PPMT test, the doctor collects a urine sample from the patient both before and after performing prostate massage. The samples are analyzed for signs of inflammation or infection. The results of the PPMT are about 90% accurate.
MRI and Ultrasound
If the doctor is unable to make a clear diagnosis of what is causing symptoms after conducting the above common tests and procedures, he or she may order further testing to get a better picture of what is going on. This may include an MRI, ultrasound, or other imaging tests. These tests are more likely to be used when the doctor suspects a case of bacterial prostatitis or believes that a bacterial prostatitis infection has spread to areas outside the prostate. The doctor may order these other imaging tests if he or she thinks that you may suffer from bladder or kidney infections, an enlarged prostate, bladder cancer, or prostate cancer.
Cystoscopy
A cystoscopy is a more invasive test. This is not as frequently used as some of the more common and less-invasive tests. The doctor may perform it to rule out structural problems. How it works is that the doctor inserts a cystoscope into the penis to view the urethra and bladder. By performing this procedure, the physician can get a sense of how hard the prostate squeezes the urethra and can see if there is residual urine left in the bladder after you urination. This procedure can help rule out a urethral stricture and see if any prostate stones are present or if there are other prostate problems such as tiny pouches, called diverticulae. Even though there is no classic appearance of prostatitis, the doctor can see structural problems that may be causing symptoms.
When you have a cystoscopy the doctor will administer local, spinal, or general anesthesia. There are a few side effects associated with cystoscopy, the most common being swelling of the urethra, which can make it harder to urinate. Bleeding can occur. Some men develop a mild urinary tract infection after the procedure, so the doctor will probably prescribe an antibiotic to prevent infection.
Uroflowmetry
Uroflowmetry is a quick and noninvasive test to measure how much urine is released and how fast it is released. This test can help the doctor determine if there is obstruction of normal urine outflow and allows him or her to see the condition and function of the lower urinary tract. Before the test, the patient may be asked to drink four glasses of water. Then he will urinate into a device that records information while he urinates.
UPOINT
UPOINT is a new system that doctors can use to make more effective treatment decisions for patients with CPPS. It was developed by a urologist to help doctors and patients customize treatment programs for managing CPPS. UPOINT stands for six domains: Urinary, Psychosocial, Organ specific, Infection, Neurologic/systemic, and Tenderness. A patient is classified as “yes” or “no” for each of the domains. This allows the doctor to see the problem areas and where the symptoms lie so he or she can provide the right kind of treatments that have proven to be effective for those problems. It can save the patient time and money because they can avoid ineffective and unnecessary treatments.
NPAT/CPPS Protocol
The NPAT/CPPS treatment protocol is a treatment program developed by a naturopathic urologist. This protocol recognizes that pain and chronic pelvic discomfort are grounded in lifestyle, diet, nutrition, and other factors that lie outside the prostate that may contribute to chronic tension. The NPAT/CPPS protocol is a holistic program that individually analyzes each patient’s symptoms to form a complete treatment program, incorporating natural and alternative remedies for prostatitis such as acupuncture, pelvic therapy, trigger point release, phytotherapy (with supplements such as quercetin and pollen extracts used with probiotics), stress management, and others.
NPAT stands for:
- Natural treatments (ALCAT, elimination diets, and wheat-free diets)
- Phytotherapy (pollen and quercetin together with probiotics)
- Alternative treatments (acupuncture, prostate massage, pelvic rehabilitation and therapy)
- Total body (exercise, chronic stress management, lifestyle)
Dr. Geo Espinosa developed the NPAT/CPPS treatment program to specifically target pelvic tension because many causes of chronic prostatitis stem from problems that take place outside of the prostate itself and elsewhere in the body. Approximately half of all cases of CPPS cases result from tension in the pelvic floor muscles and that tension can stem from stress and emotional health problems. There are a number of chronic prostatitis causes involving tension. These include pelvic floor disorders, neuromuscular tension, and chronic tension disorders. Inflammation that has origins in other places in the body usually accompanies chronic tension in the pelvic floor, and inflammation is one of the major contributors to CPPS. Immune disorders and allergies, like food intolerances, also contribute. This is why following a well-rounded whole body approach to diagnosing and treating prostatitis can help CPPS patients to reduce inflammation.
Because CPPS is nonbacterial and does not respond to treatment with antibiotics, it requires other kinds of treatment that work at helping the whole body to heal. Dealing with the ongoing pelvic pain, discomfort, and psychological effects of CPPS are very challenging for men. Only a holistic whole body approach like NPAT can offer a complete treatment that works toward regaining health and relief.
Patients who follow Dr. Geo’s NPAT program learn not only what is causing their symptoms but also how to employ treatments that target those causes. There is not one standard course to follow because each patient’s treatment is individualized to treat his specific symptoms and causes of pelvic tension. Treatments in an individual’s NPAT program might vary, but patients will generally take or follow several different natural and alternative therapies. Patients whose CPPS symptoms or flare-ups are related to diet may learn to avoid the foods that can exacerbate their symptoms like spicy foods, acidic foods, wheat, gluten, and caffeine. Other patients may learn how to better manage their stress to reduce tension. Following a multimodal approach to prostatitis is always the most successful treatment program. That is why Dr. Geo’s NPAT/CPPS treatment program works so well as a natural treatment approach while traditional treatments fail to provide relief.
Other Tests
This is not a complete list of tests for prostatitis. Your doctor may order a number of other tests to find out what is causing your symptoms, especially if other tests have not revealed the problem. If you are experiencing signs of an infection that has spread outside the prostate (e.g., chills or high fever) then you doctor may order blood cultures. Your doctor may order or perform imaging tests to help verify an infection that has spread and to look for signs of an abscess while diagnosing prostatitis. These imaging tests may include ultrasound, computed tomography, or magnetic resonance imaging (MRI). Imaging tests may also be recommended for men with recurrent urinary tract infections to help rule out kidney stones or structural problems. Throughout the diagnostic process, your doctor may use the UPOINT system to analyze the symptoms in order to customize treatment with therapies that have shown effectiveness in treating specific symptoms.
