Multiparametric MRI – What is it?
Magnetic resonance imaging (MRI) is a scanning method that uses a strong magnetic field, radio waves, and special computer software to show detailed images of organs and tissues in the body. Unlike X-rays and CT (computed tomography) scans, MRI has no radiation. It is safe and noninvasive.
MRI scans can be programmed for several different pulse sequences, or parameters, that highlight specific differences between healthy and unhealthy tissue. When two or more parameters are used, it is called multiparametric MRI (mpMRI).
How does mpMRI detect prostate cancer?
Multiparametric MRI clearly reveals prostate anatomy and anything unusual within and around it. There are four parameters that highlight different tissue characteristics in order to detect prostate cancer.
- T2 weighted MRI (T2 MRI) gives a 3D map of prostate zone anatomy.
- A suspicious-looking area is called a region of interest or ROI.
- T2 MRI is called the workhorse of prostate MRI, but more information is needed to determine if the ROI is prostate cancer or a benign (noncancerous) condition.
- Diffusion weighted imaging (DWI MRI) shows the movement of water molecules in tissue.
- Cancer cells restricts the motion more than other cells do, which shows up in DWI MRI.
- Dynamic contrast enhanced imaging (DCE MRI) reveals a tumor’s blood flow.
- A contrast agent is injected into a vein.
- Prostate cancer tumors develop their own blood vessels, which look abnormal.
- When injected, the contrast agent is quickly taken up by the tumor blood vessels, then washes out and is later excreted in urine.
- During the uptake and washout phase, the contrast agent shows the cancer’s blood flow.
- Also, the pace of the uptake/washout tells about the nature of the tumor.
- Spectroscopy (MRI-S) may be added as a fourth parameter.
- If prostate cancer is present, it maintains its life by certain chemical processes (metabolism) that are distinct from normal cell metabolism.
- MRI-S gives metabolic information that confirms prostate cancer.
What are the advantages of multiparametric over TRUS for prostate imaging?
Multiparametric MRI has significant advantages over ultrasound for prostate imaging. Ultrasound imaging uses a probe inserted into the rectum to beam sonic waves that create computer images. This is called transrectal ultrasound (TRUS). The advantages of mpMRI over TRUS include:
- Completely noninvasive – mpMRI on a powerful 3 Tesla (3T) magnet does not require a coil (antenna) inserted in the rectum, so unlike TRUS, mpMRI is completely noninvasive. NOTE: Some radiologists still prefer use of the endorectal coil, especially with less powerful magnets, but the Sperling Prostate Center and others have advanced technology that avoids the uncomfortable endorectal coil.
- Detailed 3D tumor images – mpMRI shows the prostate anatomy, and the size, shape and location of any cancerous tumor as small as .2 cc. However, TRUS is blind to tissue differences and does not reliably show tumors.
- Characterization of prostate cancer before biopsy – By combining multiple parameters, mpMRI gives advance warning about the how developed and aggressive the cancer cells are.
- Superior image guidance for interventions – Real time mpMRI is used to guide the most accurate prostate biopsy with the fewest needles, whereas TRUS guided biopsies are “blind” to tissue differences and require 12-24 needles.
Who is a candidate for Multiparametric MRI?
Multiparametric MRI of the prostate is the imaging of choice for men who
- Have a rising or abnormally high PSA – mpMRI can detect if the cause is benign or cancerous
- Are being recommended for needle biopsy – mpMRI can rule a biopsy in or out
- Have low risk prostate cancer and are considering active surveillance – mpMRI provides a baseline image as the foundation for monitoring during Active Surveillance
- Are on Active Surveillance – mpMRI will reveal any change in the cancer (e.g. more aggressive)
- Want a real-time MRI-guided in-bore biopsy with minimal needles
- Have already been treated for prostate cancer – mpMRI confirms treatment success and can monitor for recurrence outside the treatment area
What to expect during a Multiparametric MRI
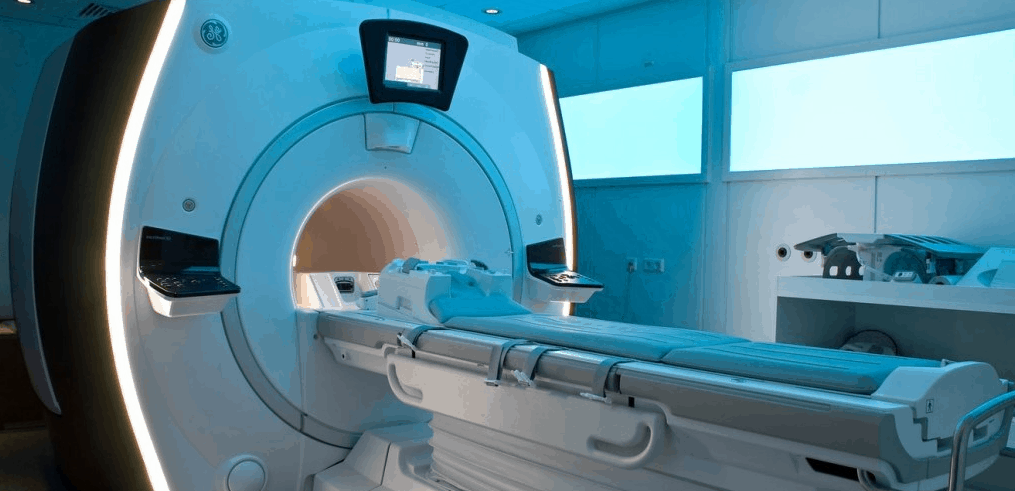
Your own doctor will prescribe the prostate MRI, and will refer you to a radiology center that has a powerful 3 Tesla (3T) magnet with the correct software.
Before the exam, the radiology center staff will provide you with their instructions. You will be required to notify the radiology center if you have any metal implants or internal devices such as a pacemaker due to possible interactions with the magnetic field, in which case you will be instructed accordingly. If you have a metal watch band, car keys, jewelry, etc. you will be given a secure place to put such items before entering the MRI.
You should let the office know in advance if you are claustrophobic (become anxious in small places) since the scan occurs in the bore, or tunnel, within the large equipment. Medication can be prescribed to help you relax completely.
You may be given a hospital gown to wear. You will then lie down on a table that can glide in and out of the MRI bore. During the scan you should avoid unnecessary movement, lying as comfortably still as possible. You will be given earplugs, since the MRI generates loud sounds. If you are having dynamic contrast enhancement, a small needle will be placed in a vein to inject the contrast agent.
There is no pain during the scan, which can take up to 30 minutes. When the scan is done, the table will glide out, and you can get dressed and leave. The radiologist will provide you and your doctor with an image CD and a thorough written report, which you should discuss with your own doctor.
Multiparametric MRI has revolutionized the prostate cancer world
High resolution mpMRI of the prostate safely provides a wealth of advance information in order to make the best next-step decisions. In a recent paper of which I was a co-author, we noted, “mpMRI reliably identifies significant disease with high sensitivity and specificity.” No other imaging available today has such accuracy in detecting prostate cancer. If something suspicious is seen, mpMRI can guide a precisely targeted biopsy of the tumor’s core. This means the fewest needles for a more accurate diagnosis.
Finally, mpMRI is used to guide precision focal treatments such as our Center’s focal laser ablation that can destroy the tumor with few to no urinary and sexual side effects. In short, mpMRI is a revolution in prostate cancer detection, diagnosis, and treatment.
Reference
Lepor H et al. Complications, recovery, and early functional outcomes and oncologic control following in-bore focal laser ablation of prostate cancer. Eur Urol. 2015 May 12. pii: S0302-2838(15)00331-0. doi: 10.1016/j.eururo.2015.04.029.