Question: What do transrectal ultrasound (TRUS) guided biopsy and MRI prostate scans have in common?
Answer: Almost nothing. While both try to find cancer in a walnut-sized gland tucked away in the pelvic bed, there’s no comparison. Noninvasive MRI detects prostate cancer better than conventional invasive TRUS biopsy. In fact, multiparametric MRI (mpMRI) is so much more accurate that it can rule out the need for a biopsy in nearly a third of men with abnormal PSA blood tests.
The problem with using a TRUS biopsy to detect prostate cancer
The current pathway for diagnosing prostate cancer involves a screening test called the prostate specific antigen (PSA) blood test. If the test is high, a TRUS biopsy is next. This method has three main problems:
- Doctors often push men into having a needle biopsy based on abnormal screening results. However, the PSA test is not specific for cancer. Other noncancerous conditions such as infection, inflammation, or gland stimulation like a digital rectal exam (DRE) or sexual activity can cause prostate cells to “shed” surface proteins (antigens) into the blood stream. Just because a blood test is unusually high does not automatically mean that cancer is the cause. But better safe than sorry, so doctors want the patient to have a biopsy.
- Unfortunately, TRUS biopsy “has poor attributes for a diagnostic test.” Ultrasound can’t distinguish tumors from normal gland tissue, so the person conducting the biopsy doesn’t know what to aim for. Biopsy needles are directed through the rectal wall into 12-14 areas, half on each side of the gland. The procedure has risks, especially infection from colon bacteria. Even when antibiotics work, many men still experience post-biopsy blood in their urine/semen.
- The TRUS biopsy approach has three inherent flaws: a) at least 30% of the results are false negatives that seem reassuring, but the cancer is still there and potentially growing; b) it overdetects insignificant prostate cancer, meaning low to very low risk disease that may never need to be treated; and c) it underdetects significant prostate cancer, which is intermediate-to-high risk and requires quick intervention.
Advantage of multiparametric MRI over TRUS biopsy for prostate cancer detection
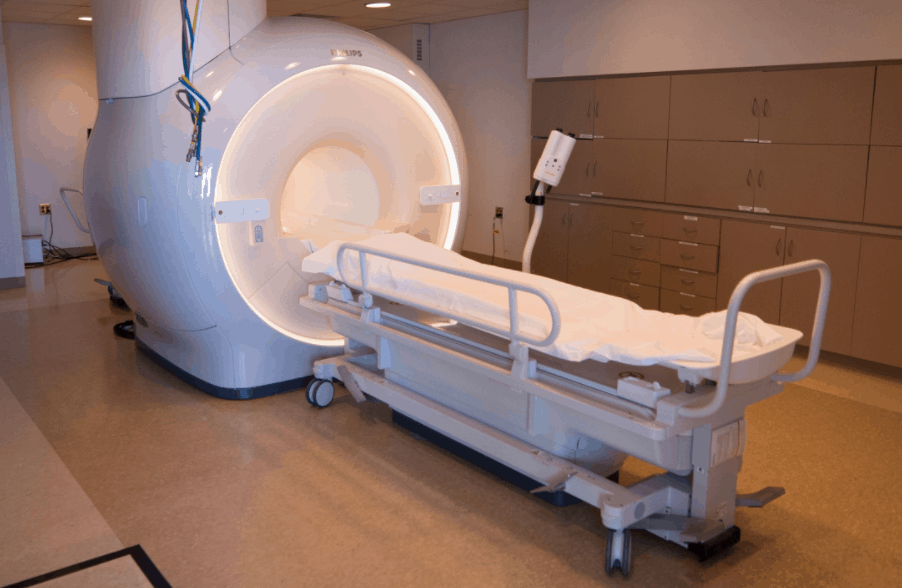
A needle biopsy is necessary to confirm prostate cancer and determine the aggression level of the disease. What’s important is that too many men who do not need biopsies are having them. This is where mpMRI comes in. If a PSA blood test sends up a red flag, and a repeat blood test shows the same results, the next step should be imaging before a biopsy. The type of imaging should be mpMRI on a magnet with high field strength (3 Tesla or 3T) for optimum resolution.
Multiparametric MRI consists of at least three imaging sequences that allow tumor analysis based on functional differences from normal tissue. Put simply, tumors are denser, less elastic, restrict the movement of water molecules, and build their own blood supply – all of which can be detected by mpMRI and correctly interpreted by an experienced reader. This means that mpMRI shows the location, size, shape and even clues regarding aggression. Ultrasound simply can’t do this.
Recent statistics from London-based prostate cancer experts showed that compared with TRUS, mpMRI had 93% sensitivity for prostate cancer in contrast to TRUS biopsy with 48%. (Sensitivity means that test correctly identified patients who actually had prostate cancer.) Even more importantly, mpMRI correctly identified over 90% of patients whose prostate cancer was significant, requiring treatment decisions.
A solution to the PSA controversy as to whether a PSA test can detect prostate cancer
There continues to be debate over the U.S. Government panel recommendation against broad PSA screening. The panel’s concern that abnormal PSA findings ultimately led to overdetection and overtreatment of insignificant prostate cancer – leaving countless men dripping urine and unable to perform sexually – seems justified due to the flaws of TRUS biopsy. New data since their first recommendation now shows that without as much screening, fewer men are being diagnosed with prostate cancer, but more men are being diagnosed with later stage, more aggressive disease that could have been picked up earlier!
More experts are recommending a return to screening but including mpMRI as the logical next step if PSA is consistently high or rising. Imaging offers a solution to the PSA dilemma because it eliminates unnecessary biopsies. Since it can detect insignificant disease, depending on other clinical factors it may be possible to simply monitor such patients on an ongoing basis using a combination of PSA tests and mpMRI. For thousands of men, this means deferring a biopsy until there is evidence of increased tumor activity.
And if a biopsy is needed, mpMRI offers one more advantage. Rather than TRUS guidance, the MRI itself can guide a real-time targeted biopsy done under MRI guidance. The precision of the imaging means a minimum number of needles can sample directly from the areas of the tumor most likely to harbor aggressive cells. Not only does this process greatly reduce the risks of prostate biopsy, but the diagnosis will give the most accurate characterization of the tumor. In turn, this means treatment can be matched and tailored to the cancer for the best chance of success with the least side effects.
Read more in our Prostate Cancer Health Center.
Reference
Hoffman J. TRUS biopsy inferior for prostate cancer detection. Prostate Cancer Advisor 2016 Jun 8